Many conditions can cause pain in the teeth. The importance of a proper diagnosis can not be overstated. Most of the time dental diagnoses are straightforward, but the exact cause of the tooth pain is not always evident. One of the difficulties doctors face in diagnosing is that patients present with a variety of pain perception, thresholds, and tolerances. However, over treatment or mistreatment can be avoided with a little proper detective work. What follows is a list of diagnoses with their usual symptoms and treatment.
Glossary
First a short vocabulary lesson would be helpful to intelligently comprehend what follows, so here is a little glossary to get you started.
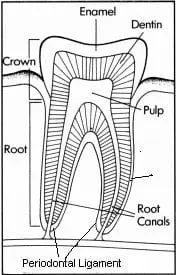
Pulp - The "nerve"...this is the living tissue inside the tooth. It has connective tissue, blood vessels, and sensory nerves.
Pulpitis - Inflammation of the pulp.
Periodontal Ligament - this structure is a series of microscopic fibers connecting the root of the tooth to the jawbone. It has very sensitive nerves designed to sense both pressure and pain.
Caries - Tooth decay. Caries is an infection of the tooth caused by specific bacteria. It is this infection which results in many of the symptoms of a toothache
Abscess - An infection characterized by a localized buildup of purulence (pus)
Enamel - Hardest part of the tooth found on the other surface of the crown. It is what you see in the mouth. Enamel is lighter in color than dentin.
Dentin - The hard part of the tooth below the enamel which surrounds the pulp chamber, most of the tooth is dentin. It has microscopic channels (pores) which can transmit both irritants and medicine to the pulp. Dentin is darker in color than enamel. It appears in the mouth as a somewhat darker or more yellowish part of the tooth between the gum and enamel.
Necrotic - means tissue has died
Conditions
- Dentin (root) Sensitivity
- Symptoms
- Cold sensitivity to liquids and sometimes air, less often to hot liquids. Short duration with no lingering or spontaneous pain. No biting pain. Root surface usually visible due to gum recession.
- Cause
- Exposed dentin (root) surface due to gum recession, trauma, teeth grinding, erosion, or abrasion
- Treatment
- Use desensitizing toothpaste for two weeks. If no resolution have dentist examine tooth to rule out decay. Dentist can treat with in office desensitizing treatments. Dental restoration may be needed if tooth has lost tooth structure. Usually responds to treatments though some teeth can be very resistant to therapies.
- Symptoms
- Reversible Pulpitis
- Symptoms
- Cold sensitivity to liquids and sometimes air, less often to hot liquids. Short duration with no lingering or spontaneous pain. No biting pain. Cavity in tooth may or may not be visible to the patient.
- Cause
- Decay - byproducts of the decay infection irritate the nerve, though the pulp itself is not infected by the bacteria. At this point the germs are in the dentin only.
- Treatment
- The dentist fills your tooth and the decay is meticulously removed.
- Symptoms
- Irreversible Pulpitis
- Symptoms
- Severe temperature sensitivity which often lingers for minutes or more. Spontaneous, throbbing pain is often present as well, sometimes causing sleep difficulties. Pain killers like Tylenol or aspirin may be needed. Biting pain is usually not present but will present on occasion or as tooth becomes more infected. Visible decay may or may not be present.
- Cause
- Infection of the pulp secondary to a cavity in the tooth. The bacteria has penetrated beyond the dentin and now inhabits the pulp. Eventually the nerve will die and become necrotic, hence the irreversible nature of this condition.
- Treatment
- Root canal or extraction
- Symptoms
- Necrotic (Dead) Tooth
- Symptoms
- Pain from irreversible pulpitis may subside almost completely. Eventually the tooth may abscess where the infection of the pulp leaks from the tooth into the jaw bone below. At this point the pain can become quite severe. Biting pain is evident, often resulting in avoidance.Swelling may arise in the tissues adjacent to the tooth. Left untreated this swelling can become visible on the patients face. At this point fever, swollen lymph nodes, and malaise may occur. General sepsis and/or swelling of dangerous areas may result, resulting in a true emergency.
- Cause
- Bacteria from the infected pulp infiltrate the jaw bone.
- Treatment
- Root canal or extraction. Additional surgical intervention is sometimes needed to drain the infection. Antibiotics are sometimes indicated.
- Symptoms
- Cracked Tooth Syndrome
- Symptoms
- Occasional cold sensitivity is sometimes present. Pain on biting hard foods (pretzels, carrots, etc.) is the hallmark of the condition. This biting pain is inconsistent and usually occurs when the involved cusp is contacted in a certain way. The involved tooth can be difficult to localize.
- Cause
- A hairline fracture in tooth caused by trauma, grinding/ clenching habits, and the like. Biting on hard food causes the crack to open and close slightly irritating the pulp. Cold may more readily transmitted to the pulp as well. Decay is often found along the fracture deep in the tooth contributing to the symptoms via a reversible pulpitis (see above). Cracked tooth syndrome can be confirmed by your dentist doing a bite test and examining the tooth with a fiber optic transilluminator, a bright light which shows fractures.
- Treatment
- A crown effectively splints the tooth, eliminating symptoms in most cases. Sometimes a root canal is needed to treat teeth not resolved by the crown alone
- Symptoms
- Occlusal (Bite)Trauma
- Symptoms
- This condition can mimic any of the above conditions. The tooth may be sensitive to cold and/or biting. The tooth may be achy and sore to the touch
- Cause
- Occlusal trauma is caused when the bite is excessive on an individual tooth or teeth. Recent dental work is a common cause. The bite on a tooth often looks good to the dentist and feels fine to the patient initially, but is just high enough to cause a problem. Other scenarios is when a tooth drifts into an unfavorable position, an increase in tooth grinding, or other bite changes. This pain originates in the ligament around the tooth and leads to internal pulpal inflammation as well.
- Treatment
- Adjustment of the bite on the offending tooth. The T Scan III computerized bite analyzer has been a tremendous aid in diagnosing these teeth.
- Adjustment of the bite on the offending tooth. The T Scan III computerized bite analyzer has been a tremendous aid in diagnosing these teeth.
- Symptoms
- Periodontal Abscess
- Symptoms
- Dull to severe ache around a tooth or teeth. Swelling of the gums and/ or pus formation may be present. Temperature sensitivity not usually a problem. Tooth may feel loose, accompanied by a bad taste in the mouth and bad breath (halitosis).
- Cause
- Acute infection secondary to periodontitis(gum disease).
- Treatment
- Localized drainage and scaling and Antibiotics indicated in more severe cases.
- Symptoms
Conditions Which May Mimic a Toothache
- Temporomandibular Disorder
- Bruxism
- Sinusitis
- Trigeminal Neuralgia
- Atypical Facial Pain
- Heart Attack
- Tumors

